Abstract
Bronchopulmonary dysplasia (BPD) is a chronic lung disease typical of preterm infants. It is associated with high morbidity and risk of short- and long-term mortality. Despite improvements in perinatal care, its incidence has remained relatively constant: it occurs in 40-45% of infants born before the 29th week of gestation.
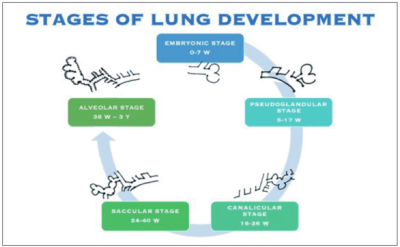
Current definitions of this disease show several limitations, and this could be linked, in particular, to its multifactorial pathogenesis. Today, BPD occurs more commonly in extremely preterm infants, and it is characterized by a milder but longer course, mainly due to the extreme immaturity of the lungs at birth, with arrested maturation in the canalicular or early saccular stage, interruption of alveolarization, altered and dysregulated microvascular development, high pulmonary vascular resistance, and abnormal vascular reactivity.
The pathogenesis of BPD is multifactorial: prolonged exposure to high oxygen levels, the lung damage caused by mechanical ventilation, the inflammatory state and, last but not least, the epigenetic/genetic risk factors. Further investigations concerning BPD pathogenesis showed that extremely preterm birth is associated with significative dysbiosis in airway microbiome.
In the future, metabolomics, thanks to its ability to identify instant variations of metabolites possibly related to disorders, could help to recognize those associated with BPD and its pathways alterations.